eISSN 2444-7986
DOI: https://doi.org/10.14201/orl.29553
REVIEW
MAXILLARY SINUS PATHOLOGY AND ITS RELATIONSHIP WITH PATHOLOGY AND DENTAL TREATMENTS. SYSTEMATIC REVIEW
Patología del seno maxilar y su relación con la patología y los tratamientos dentales. Revisión sistemática
María AREIZAGA-MEDINA  1; Beatriz PARDAL-PELÁEZ
1; Beatriz PARDAL-PELÁEZ  2; Javier MONTERO
2; Javier MONTERO  3
3
1DDS.PhD student. University of Salamanca. Salamanca. Spain.
2DDS, PhD. Associate Professor. Faculty of Medicine. Dental Clinic. Department of Surgery. University of Salamanca. Salamanca. Spain.
3DDS, PhD. Lecturer of Stomatological Prosthesis. Faculty of Medicine. Dental Clinic. Department of surgery. University of Salamanca. Salamanca. Spain.
Correspondence: bpardal@usal.es
Reception date: June 13, 2022
Date of Acceptance: July 18, 2022
Publication date: July 20, 2022
Date of publication of the issue: March 24, 2023
Conflict of interest: The authors declare no conflicts of interest
Images: The authors declare that the images have been obtained with the permission of the patients
Rights policy and self-archive: the self-archive of the post-print version (SHERPA / RoMEO) is allowed
License CC BY-NC-ND. Creative Commons Attribution-Noncommercial-NoDerivate Works 4.0 International
University of Salamanca. Its commercialization is subject to the permission of the publisher
SUMMARY: Introduction and objective: The aim of this review is to evaluate to what extent sinus pathology originates from dental pathology or treatment, and to assess the occurrence frequency of sinus pathology in its different forms using cone beam computed tomography (CBCT). Method: The literature review was conducted using PubMed, Scopus and the Cochrane Library. Forty-two articles were included (25 case series, ten cross- sectional studies, three case-control studies, two cohort studies, one prospective study, and one retrospective study). Results: Forty-two articles involving a total of 13,191 patients and 17,374 CBCTs were included in this review. The most frequent pathological findings were, by a considerable degree, inflammatory diseases, which represented 75.16 % of the total findings, followed by infection (12.13 %), tumours (6.88 %), and high pneumatisation (2.07 %). Within dental pathology, there is a direct Pearson correlation with polyps (1) and opacification (0.999), and an almost direct correlation with retention cysts (0.981) and sinus-associated dental elements (0.972). Conclusions: Our results further support the argument that dental modifications and treatments are an important cause of sinus pathology. For this reason, dental aetiologies must be taken into account by both dentists, maxillofacial surgeons and ENT when considering the most appropriate treatment for patients with maxillary sinusitis.
KEYWORDS: maxillary sinus; pathology; dental care; systematic review.
RESUMEN: Introducción y objetivo: El objetivo de esta revisión fue evaluar en qué medida la patología sinusal se origina a partir de patología o tratamiento dental, y evaluar la frecuencia de aparición de la patología sinusal en sus diferentes formas mediante tomografía computarizada de haz cónico (CBCT). Método: Se realizó una búsqueda bibliográfica utilizando PubMed, Scopus y Cochrane Library. Se incluyeron 42 artículos (25 series de casos, diez estudios transversales, tres estudios de casos y controles, dos estudios de cohortes, un estudio prospectivo y un estudio retrospectivo). Resultados: En esta revisión se incluyeron 42 artículos con un total de 13191 pacientes y 17374 CBCT. Los hallazgos patológicos más frecuentes fueron, en grado considerable, las enfermedades inflamatorias, que representaron el 75,16 % del total de hallazgos, seguida de la infección (12,13 %), los tumores (6,88 %) y la neumatización (2,07 %). Dentro de la patología dental, existe una correlación directa de Pearson con los pólipos (1) y opacificación (0,999), y una correlación casi directa con quistes de retención (0,981) y elementos dentales asociados al seno (0,972). Conclusiones: Los resultados obtenidos respaldan el argumento de que las patologías y tratamientos dentales son una causa importante de patología sinusal. Por este motivo, tanto los odontólogos como los cirujanos maxilofaciales y otorrinolaringólogos deben tener en cuenta las etiologías dentales a la hora de considerar el tratamiento más adecuado para los pacientes con sinusitis maxilar.
PALABRAS CLAVE: seno maxilar; patología; cuidado dental; revisión sistemática.
INTRODUCTION
ANATOMY AND PHYSIOLOGY OF THE MAXILLARY SINUS
The maxillary sinus is a bilateral air cavity that occupies the body of the maxilla. It is internally limited by a thin mucous membrane of ciliated respiratory epithelium that is continuous with the nasal epithelium 1]. The drainage ostium of the maxillary sinus opens to the nose through the infundibulum at the level of the middle meatus. The maxillary sinus is drained as a result of the activity of the cilia and the negative pressure produced in the sinus during inspiration. This cavity has several functions: a respiratory function for heating the air that is breathed in; defence and protection against bacterial and viral invasion; resistance to mechanical shocks; and a vocal function, as it acts as a resonant cavity that supports and amplifies the emission of laryngeal sound [2].
WHAT IS THE RELATIONSHIP BETWEEN THE ANTRAL TEETH AND THE SINUS?
Modifications of the sinus mucosa as a consequence of dental pathology result from the intimate anatomical relationship that some teeth have with the floor of the maxillary sinus [3]. The roots of the posterior maxillary teeth are separated from the sinus by a variable thickness of cortical bone and there are also numerous vascular anastomoses that perforate this space and can serve as channels for the propagation of bacteria, facilitating the spread of odontogenic infections towards the maxillary sinus [4].
The teeth most frequently related to the sinus are the first and second upper molars, followed by the premolars, whose relationship depends on the size of the molar and its degree of pneumatization [5]. Furthermore, these teeth tend to have a high prevalence of periapical lesions compared to others, particularly those teeth that have been treated endodontically, in addition to a greater susceptibility to periodontal disease due to dental furcation involvement [3, 4]. This explains why 30 % of maxillary sinusitis cases are dental in origin. In addition, maxillary sinusitis is the most frequent complication after invasive dental treatments (up to 27 %), although the diagnostic criteria are not always straightforward [6].
WHICH DENTAL PATHOLOGIES MAY BE RELATED TO SINUS PATHOLOGY?
Sinusitis of dental origin should be considered in patients presenting symptoms of maxillary involvement who have a previous history of dental infection, dentoalveolar surgery, periodontal pathology, endodontics related to antral teeth, sinus elevations, implants, and those cases resistant to conventional treatment [5, 6].
Odontogenic sinus infections tend to have higher microbiological loads with a high predominance of anaerobic microorganisms. Their clinical characteristics are similar to those of non-odontogenic sinusitis, but they are generally unilateral and not necessarily associated with ostium obstructions [3]. The diagnosis of odontogenic sinus pathologies must, therefore, be multidisciplinary, and a clinical assessment must be complemented by other techniques, such as imaging [6].
WHAT TYPES OF IMAGING TESTS CAN BE PERFORMED TO EVALUATE THE SINUS? WHAT IS THE GOLD STANDARD?
X-rays and clinical dental evaluations are unable to detect antral teeth infections that may cause odontogenic sinusitis. Panoramic x-rays are the most typical two- dimensional image projections used by the majority of dentists to make a general evaluation of the orofacial complex, allowing them to determine the size of an apical lesion, visualise cysts, and evaluate the relationship between the teeth and the sinus floor. They do, however [7], have inherent limitations. In addition, cancellous bone lesions cannot be consistently detected with these radiographic techniques. In the maxilla, the degree the antral roots protrude into the maxillary sinus tends to be overestimated. Another drawback is that the soft tissues of the sinus cannot be viewed effectively [8].
Computed tomography (CT) used to be considered the gold-standard for sinus imaging, although it does have disadvantages when compared to cone beam computed tomography (CBCT), including: greater radiation exposure, and an increased likelihood of generating artifacts when hyperdense materials are present near the area of interest. For this reason, CBCT is now the procedure of choice both for the preoperative evaluation of the maxilla, and to assess sinus health status or pathology [9].
WHICH SINUS DISEASES MAY BE RELATED TO DENTAL PATHOLOGY?
The intimate relationship between the maxillary sinus and the roots of the teeth makes it possible for symptoms originating in the sinus to manifest at the dental level and vice versa. Physiologically, the roots of the teeth are separated from the maxillary sinus by a thin, sometimes non-existent, layer of cortical bone and a mucoperiosteum of variable thickness, which may explain how the sinus inflammation develops [7]. Pathological symptoms of inflammation are common in the maxillary sinus, including mucosal thickening, polypoid lesions, sinus opacification, and hydro-aerial level. The aetiology is varied, it may be secondary to inflammatory and infectious processes, such as periodontal disease, root and dental cysts, endodontic infections, retained teeth, iatrogenic causes, or extractions closely associated with the sinus [10].
Due to the difficulty of differentiating symptoms of dental and sinus origin, a detailed dental history of pathology, symptoms, previous surgeries, treatments, and trauma must be compiled, in addition to radiological studies. Both extraoral and intraoral examinations and complementary tests are also required to ensure a precise diagnosis [11].
JUSTIFICATION AND OBJECTIVE
Despite the fact that dental pathology is recognised as causing some sinus disorders, there is little literature on how to manage this in the scope of dentistry, as 90 % of the published work comes from the field of otorhinolaryngology [7]. Due to the increase in dental procedures and related diagnostic tests, this percentage may now be rising.
The primary objective of this study was, therefore, to determine how much sinus pathology originates from dental pathology or treatment. The secondary goal was to evaluate the frequency with which sinus disease appears in its various forms, by means of a CBCT study.
To this end, the following PICO question was applied: Patients –patients attending an ear, nose and throat (ENT) or dental assessment–; Interventions –CBCT–; Comparison –sinus pathology of oral origin vs. sinus pathology of non-oral origin–; Outcome –how much dental pathology is related to sinus pathology–. In patients who come for an ENT or dental check-up (Patients), who have a CBCT (Interventions) and who have sinus pathology associated or not with antral teeth (Comparison), is it possible to evaluate how much dental pathology is directly related to sinus pathology (Outcome)?
MATERIAL AND METHODS
ELIGIBILITY CRITERIA
Inclusion criteria. We incorporated the articles in English and Spanish that included the abstract and in which the pathology of the maxillary sinus was studied by means of imaging techniques (CBCT, panoramic x-ray or Waters). We included patients who attended their ENT service for sinus disease as well as those who attended their dental service for dental treatment with or without known dental or sinus disease. Meta-analyses, systematic reviews, clinical trials, prospective, and retrospective studies were reviewed.
Exclusion criteria. Papers investigating anatomical variations of the maxillary sinus or other paranasal sinuses, as well as systemic pathologies or those involving microbiology of the maxillary sinus were excluded. Articles that did not include radiological studies of the sinus were also excluded. Clinical cases were rejected.
INFORMATION SOURCES AND SEARCH
Three online databases, PubMed, Cochrane Library and Web of Science, were searched extensively without time constraints.
All types of articles were selected except for clinical cases, due to the scarcity of works in this regard, due to the scarcity of papers on the subject. There are no randomized clinical trials, so most of them are observational since they are studies with findings observed in radiology. No screening by type of article or quality criteria was performed, as it was considered that relevant information could be lost.
The complete search strategy is shown below and is specified in the flow chart following the PRISMA criteria [12] (Figure 1). The last bibliographic search was carried out on 25/02/2020.
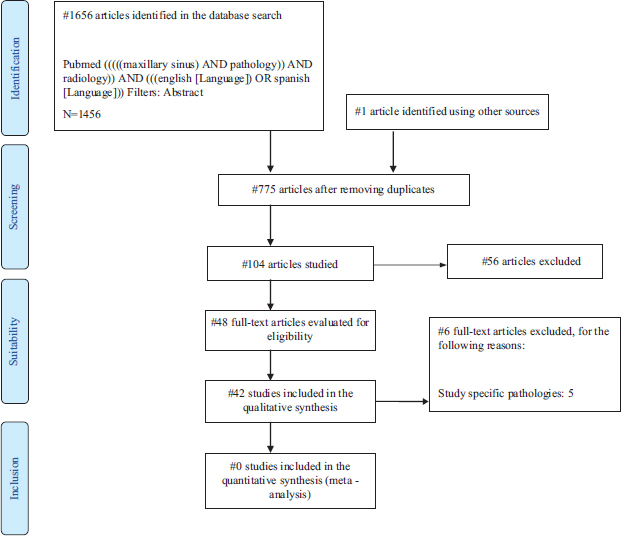
Figure 1. Flowchart of the included studies.
DIAGRAM DESCRIPTION
The initial search strategy used the following combinations of terms: maxillary sinus AND pathology AND radiology. These terms were adjusted according to the requirements of each electronic database. In the three databases used, 1656 articles were identified. In addition, one study identified via other sources was included [13]. Inclusion and exclusion criteria were applied, and after eliminating duplicates, 48 publications were identified as suitable for inclusion as full texts. After reading this series of publications, 6 articles were excluded for the following reasons: study of specific sinus pathologies [14-18] and due to the absence of data in the article and the fact these could not be obtained by contacting the author [19]. Finally, 42 studies were included in the qualitative analysis.
STUDY SELECTION
Data extraction process and data list
The data extracted from each of the studies are detailed below: number of patients, age and sex, diagnostic imaging (CBCT or panoramic x-ray), and number of maxillary sinuses (pathological and physiological). Sinus findings were collected (mucosal thickening, opacification, mucocele, hypoplasia, silent sinus, retention cyst, malignant and benign tumours, polyps, sinusitis, pneumatisation, sinus-associated dental elements, antroliths, fungal infection, ostium obstruction, foreign body, aplasia, and fluid). Dental pathology and general treatments, pre-implant (sinus lift) and post- implant dental treatments were also recorded.
SYNTHESIS OF RESULTS
Of the 42 articles studied, data were extracted on the different sinus pathologies found, as well as the pathology or dental treatment associated with the pathological sinuses. Firstly, a descriptive analysis of the results obtained was carried out in Excel to ascertain the prevalence of the variables mentioned above.
Next, a quantitative parametric inferential analysis was conducted using JAMOVI software (The jamovi Project (2020) jamovi (1.2 version)), by means of the T-student test, as well as various correlations between sinus pathology, pathological sinuses and dental pathology or treatment. To study the correlations, the Pearson linear correlation coefficient was used, which is the most convenient for detecting possible relationships/associations between continuous (numerical) variables. This value can range from -1 to +1, the latter being indicative of a perfect linear relationship; values close to 0 are associated with independence, the null hypothesis in this type of contrast. The results are expressed with their confidence interval with an accuracy of 95 % (CI 0.95), and a standard error of 5 % (0.05).
Due to the high heterogeneity of the data, it was not possible to perform a meta- analysis of the prevalence of sinus pathology related to dental pathology.
RESULTS
STUDY SELECTION AND CHARACTERISTICS
Forty-two articles were selected in which 13,191 patients were examined and 17,374 CBCTs were performed, for dental reasons in 71 % of cases (9,431/13,191) and for ENT purposes in 29 % (3,760/13,191). Of the selected articles, 25 (59.52 %) were case series, 10 (23.82 %) were cross-sectional studies, 3 (7.14 %) case-controls, 2 (4.76 %) cohort studies, 1 (2.34 %) prospective study, and 1 (2.34 %) retrospective study.
Of the 13,191 patients studied, disease was found by chance in 13.05 % (1,721/13,191), while symptoms were present in 34.36 % (4,533/13,191). The other cases were not chance, but it is not specified whether the patients were symptomatic or not in 86.95 % of the cases (11,470/13,191).
RESULTS OF INDIVIDUAL STUDIES
Table 1 (Appendix 1) presents the characteristics of the types of studies included and their duration, detailing the number of pathological or physiological sinuses, as well as pathology and dental treatment.
Figure 2 shows the prevalence of physiological maxillary sinuses 66.26 % (16,918/25,533) and pathological maxillary sinuses 33.74 % (8,615/25,533) with respect to total sinuses studied (25,533).

Figure 2. Prevalence of physiological maxillary sinuses and pathological maxillary sinuses with respect to the total number of sinuses studied.
Figure 3 shows the distribution of sinus findings broken down, the most frequent being mucosal inflammation with 42,70 % followed by mucosal thickening 41.50 % and infection with 10,86 %. Absent sinus findings were high pneumatization, mucocele, silent sinus, aplasia and pneumatization.

Figure 3. Detailed distribution of sinus findings.
Table 2 shows the 17 articles that related dental and sinus pathology. As can be seen, within dental pathology (2,495), periapical inflammatory cysts were found in 54.19 % (1,352/2,495) of cases, followed by periodontal disease/bone loss in 34.91 % (871/2,495).
Table 2. Dental pathology associated with the maxillary sinuses studied.
AUTHOR/YEAR |
TOTAL No. SINUSES STUDIED |
TOTAL DENTAL PATH |
PERIODONTAL DIS./BONE LOSS |
PERIAPICAL CYST |
DENTAL CARIES |
OTHER |
Aksoy et al., 2018 |
588 |
224 |
No data |
224 |
No data |
No data |
Bajoria et al., 2019 |
1,000 |
128 |
60 |
17 |
47 |
4 |
Bornstein et al., 2018 |
268 |
18 |
10 |
8 |
No data |
No data |
Connor et al., 2000 |
330 |
0 |
No data |
No data |
No data |
No data |
Dorothea et al., 2013 |
76 |
17 |
17 |
No data |
No data |
No data |
Drage et al., 2013 |
584 |
115 |
No data |
15 |
No data |
100 |
Goller-Bulut et al., 2015 |
410 |
159 |
No data |
159 |
No data |
No data |
Horwitz et al., 2017 |
162 |
23 |
No data |
23 |
No data |
No data |
Kawai et al., 2018 |
338 |
19 |
8 |
11 |
No data |
No data |
Maillet et al., 2011 |
164 |
100 |
No data |
100 |
No data |
No data |
Nascimento et al., 2016 |
766 |
589 |
254 |
335 |
No data |
No data |
Nunes et al., 2015 |
321 |
92 |
No data |
92 |
No data |
No data |
Phothikhun et al., 2012 |
500 |
539 |
500 |
39 |
No data |
No data |
Pokorny et al., 2013 |
33 |
24 |
9 |
15 |
No data |
No data |
Tassoker et al., 2019 |
400 |
141 |
No data |
141 |
No data |
No data |
Terlemez et al., 2019 |
570 |
157 |
No data |
157 |
No data |
No data |
Troeltzsch et al., 2015 |
174 |
150 |
13 |
16 |
No data |
121 |
TOTAL |
6,684 |
2,495 |
871 |
1,352 |
47 |
225 |
Figure 4 shows the distribution of sinus findings broken down, the most frequent being mucosal thickening with 60.65 % (6132/10111), followed by sinusitis 11.20 % (1132/10111) and retention cyst and mucocele with 5.46 % (552/10111).
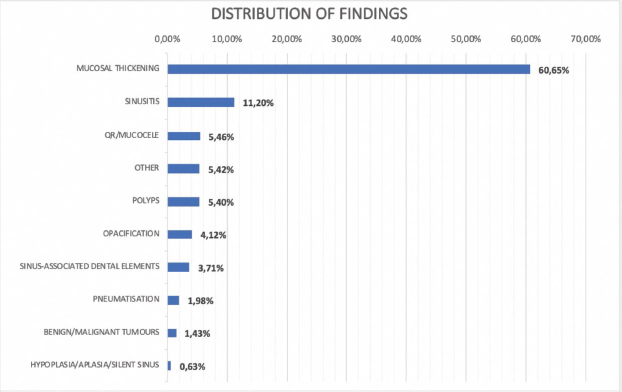
Figure 4. Distribution of sinus findings with respect to maxillary sinuses presenting dental pathology.
Table 3 shows the number of dental pathologies and treatments found, as well as the sum of these in relation to the number of teeth studied (5,558) in the articles that examined one or more teeth per patient.
Table 3. Relationship between number of teeth with pathology and dental treatment.
AUTHOR |
DENTAL PATHOLOGY |
DENTAL TMT |
SUM DP-DT |
No. TEETH (relation to the pathology, dental tmt) |
Aksoy et al., 2018 |
224 |
143 |
367 |
1,720 |
Bajoria et al., 2019 |
132 |
197 |
329 |
No data |
Bornstein et al., 2018 |
18 |
3 |
21 |
25 |
Connor et al., 2000 |
0 |
192 |
192 |
No data |
Dorothea et al., 2013 |
17 |
No data |
17 |
No data |
Drage et al., 2013 |
120 |
No data |
120 |
No data |
Goller-Bulut et al., 2015 |
159 |
No data |
159 |
1,169 |
Horwitz et al., 2017 |
23 |
No data |
23 |
No data |
Kawai et al., 2018 |
19 |
12 |
31 |
No data |
Maillet et al., 2011 |
100 |
21 |
121 |
534 |
Nascimento et al., 2016 |
580 |
234 |
814 |
No data |
Nunes et al., 2015 |
92 |
No data |
92 |
No data |
Phothikhun et al., 2012 |
539 |
21 |
560 |
No data |
Pokorny et al., 2013 |
24 |
No data |
24 |
No data |
Tassoker et al., 2019 |
141 |
No data |
141 |
400 |
Terlemez et al., 2019 |
157 |
112 |
269 |
1,710 |
Troeltzsch et al., 2015 |
150 |
150 |
300 |
No data |
TOTAL |
2,495 |
1,085 |
3,580 |
5,558 |
Dental tmt; Dental treatment, Sum DP-DT; Sum of pathology and dental treatment |
||||
SYNTHESIS OF RESULTS
The general correlations between the different sinus pathologies with the number of maxillary sinuses, pathological sinuses and dental pathology are described below. The H0 established shows that there is no relationship between the previously mentioned variables, while the Ha indicates the existence of a relationship between them. For the total number of maxillary sinuses with clustered findings, using Pearson's linear correlation coefficient it can be seen that there is a practically direct association with inflammation (0.992), tumours (0.973), infection (0.951), and low pneumatisation (0.814). Among the inflammatory findings, mucosal thickening (0.988), opacification (0.975), and retention cyst (0.960) stand out. The number of pathological maxillary sinuses shows practically the same degree of high linear correlation as described above. Within dental pathology, direct correlation is observed with polyps (1) and opacification (0.999) and there is practically a direct correlation with retention cyst (0.981) and with sinus-associated dental elements (0.972). From the data available, we observed a significant positive relationship between inflammatory cases (0.526) and benign tumours (0.598). Furthermore, there is little inverse relationship between infectious findings (-0.064) and antroliths (-0.273).
Table 4 (Appendix 2) presents the sinus findings grouped into subgroups; inflammation included mucosal thickening, opacification, ostium obstruction, mucocele, and polyps. We also included sinusitis and fungal infection in the infection findings. Tumours were subsequently grouped into malignant, benign, and retention cyst. Low pneumatisation included silent sinus, hypoplasia and aplasia, while high pneumatisation included the data related to pneumatisation. The foreign body group included foreign bodies and antroliths. Finally, symptoms and iatrogeny were grouped together.
DISCUSSION
SUMMARY OF THE EVIDENCE
Maxillary sinusitis is a pathology that, although traditionally viewed as falling within the field of otolaryngology, often involves the participation of dentists, in both diagnosis and prevention [7]. Some researchers have studied the frequency of odontogenic maxillary sinusitis and have presented various treatment methods. However, the information available from a dental perspective is limited, and it is likely that the information in the literature on the incidence of maxillary sinusitis of dental origin is an underestimate [20].
Forty-two articles were included in this review (25 case series [21-45], 10 cross- sectional studies [13, 46-54], 3 case-control studies [55-57], 2 cohort studies [58-59], 1 prospective study [60], and 1 retrospective study [61]). It involved a total of 13191 patients and 17374 CBCTs. The most frequent pathological findings were, by a considerable degree, inflammatory diseases, which represented 75.16 % of the total findings, followed by infection (12.13 %), tumours (6.88 %), and high pneumatisation (2.07 %). Finally, iatrogenic findings, the presence of a foreign body, low pneumatisation and symptoms occurred with a frequency of less than 2 %.
For inflammation, the most frequent finding was the thickening of the mucosa of the maxillary sinus (60.65 %). Of the 42 studies included in this review, 33 found mucosal thickening, with a mean frequency of 69.34 % (range 13.04-100.00 %). In 500 subjects undergoing CBCT tests, Almeida Da Silva et al. [46] observed that most pathological findings were classified as mucosal thickening, representing almost 80 % of the sinus pathology encountered. Connor et al. [41] reviewed 330 CT images of the maxillary sinus in 165 patients to determine whether the presence of dental restoration might predispose to maxillary sinusitis and, in particular, to focal thickening of the maxillary sinus mucosa as a characteristic of dental origin. They found that focal thickening of the sinus mucosa, with or without evidence of rhinogenic aetiology, occurred significantly more frequently in the sinus adjacent to dental restoration. However, the incidence of general pathology in the adjacent maxillary sinus was not significantly different from that in the sinus not adjacent to the dental restoration. These findings suggest a relationship between focal thickening of the maxillary sinus mucosa and the presence of dental restoration, which is likely to be due to an associated dental pathology. For that reason, dental restoration should be identified through a clinical exam and a CT scan, as it is a potential aetiological factor for sinusitis of dental origin. This study found a 37.5 % prevalence of mucosal thickening on CBCT images [46]. Similar results were also observed by Ritter et al. who reported a 38.1 % prevalence of mucosal thickening in a CBCT imaging study of 1029 patients [53].
Of the 42 studies analysed here, 17 related maxillary sinus pathology to dental conditions and, specifically, 7 studies [21, 26, 29, 41, 49, 56, 59] found an association between mucosal thickening of the maxillary sinus and dental modifications.
Aksoy et al. [21] retrospectively evaluated the thickening of the maxillary sinus mucosa and its relationship with dental conditions using CBCT imaging in a total of 294 patients and involving 588 maxillary sinuses. In 172 patients (58.5 %) they found mucosal thickening of more than 2 mm, which was considered the pathological threshold, in one or both maxillary sinuses. In addition, the prevalence of pathological mucosal thickening for maxillary sinuses with and without periapical lesions was 42.1 % and 53.6 %, respectively (p<0.05), and this increased significantly (p<0.05) in patients with alveolar bone loss. On this basis, they concluded that multiple conditions, including periapical infections, endodontics, and the close relationship of the maxillary teeth with the sinuses, may have a precursor effect on the appearance of maxillary sinus mucosa thickening. Consequently, the periodontal status and its role as a risk factor for triggering sinus infections should be considered not only by dentists, but also by medical professionals to establish the treatment of maxillary sinus injuries.
Connor et al. [41] reviewed 330 CT images of the maxillary sinus in 165 patients to determine whether the presence of dental restoration might predispose to maxillary sinusitis and, in particular, to focal thickening of the maxillary sinus mucosa as a characteristic of dental origin. They found that this thickening of the sinus mucosa, with or without evidence of rhinogenic aetiology, occurred significantly more frequently in the sinus adjacent to dental restoration. However, the incidence of general pathology in the adjacent maxillary sinus was not significantly different from that in the sinus not adjacent to the dental restoration. These findings suggest a relationship between localised thickening of the maxillary sinus mucosa and the presence of dental restoration, which is likely to be due to an associated dental pathology. For that reason, dental restoration should be identified through a clinical exam and a CT scan, as it is a potential aetiological factor for sinusitis of dental origin.
Nascimento et al. [26] evaluated the most common types of maxillary sinus disorder (generalised and localised mucosal thickening, maxillary sinusitis, and retention cysts) and their association with dental conditions (inadequate endodontic treatment, periapical lesions and periodontal bone loss) in CBCT images of 400 patients with disease in one or both maxillary sinuses. The most prevalent sinus pathologies were generalised (65.2 %) and localised (24.8 %) mucosal thickening, which were also the only ones related to dental conditions (periodontal bone loss and periapical lesions, respectively).
The case series study by Dagassan-Berndt et al. [56], based on CBCT images, looked at the presence of maxillary sinus mucosa thickening in two groups of patients with advanced dental pathology: 17 patients scheduled for maxillary molar surgery who underwent a CBCT for preoperative diagnosis (dentate group) and 21 patients who required a CBCT for the insertion of an implant in the posterior maxilla and who served as controls (edentulous group). The thickness of the sinus mucosa was significantly greater in the dentate group than in the edentulous group, both in the first molar position (p=0.028) and in the second (p<0001). In addition, periapical lesions(p=0.008) and the distance between the tooth apices and the maxillary sinus (p=0.036) was significantly associated with the thickness of the maxillary sinus membrane.
In our review, the dental modifications that were most frequently related to sinus pathology were periapical inflammatory cysts (54.19 %) and periodontal bone loss (34.91 %). Other systematic reviews and meta-analyses [7] have also investigated the aetiologies of maxillary sinusitis and its relationship with dental pathology, with mixed results.
Furthermore, the review by Terlemez et al. [59] described the fact that anatomically associated periapical lesions of the maxillary sinus, seen on CBCT images, were a risk factor (OR: 2.7; p<0.05) for mucosa thickening.(59) The retrospective study by Goller- Bulut et al. [49] looked at the relationship between maxillary sinus mucosa thickness and periodontal bone loss with related periapical tooth conditions, as well as the association between the tooth apices and the lower wall of the maxillary sinus, in CBCT images of 250 patients, involving 410 maxillary sinuses. They found a significant correlation between mucosal thickness and the severity of bone loss and apical lesions. Phothikhun et al. [29] also observed an association between the severity of periodontal bone loss, as assessed by CBCT, and mucosal thickening of the maxillary sinus (OR: 3.02; p<0.001), but no association was found with periapical lesions.This is consistent with the results of our review which revealed mucosal thickening to be the most frequent disease (60.65 %) in the studies analysed, while retention cysts and opacification accounted for only 5.46 % and 4.12 % of the total findings, respectively.
Arias-Irimia et al. [7] found iatrogeny to be the most frequent cause (55.97 %) of odontologenic maxillary sinusitis. Other possible aetiologies were periodontitis (40.38 %) and odontogenic cysts (6.66 %). The most prevalent iatrogenic causes were oroantral fistulas and root remains, taken together as iatrogeny after dental extraction, which accounted for 47.56 %, while dressings for closing these oroantral fistulas and non-specific foreign bodies constituted 19.72 %, and extrusion of filling materials for endodontics in the maxillary sinus represented 22.27 %. These results are not in line with the findings of our review, which showed that iatrogenic findings were very rare, making up only 1.78 % of the total number of pathological findings observed.
Pearson’s correlation analysis of the number of pathological maxillary sinuses revealed very high and significant associations with inflammation (r=0.992, p<0.001), tumour (r=0.976, p<0.001), infection (r=0.949, p<0.001), and low pneumatisation (r=0.879, p=0.021). In the case of inflammation, the most important correlations were with mucosal thickening (r=0.898, p<0.001), opacification (r=0.978, p<0.001), and retention cysts (r=0.971, p<0.001). For dental pathology, direct correlations were observed with polyps (r=1.000; p=0.007), and opacification (r=0.999; p<0.00), and practically direct correlations were seen with retention cysts (0.981; p<0.00) and sinus-associated dental elements (r=0.972; p=0.006). Finally, when we analysed the correlations between sinus pathology and the sum of pathology and dental treatment, we observed a positive and significant association with inflammatory findings (r=0.526; p=0.044) and, specifically, with sinus mucosa thickening (r=0.536; p=0.040). In contrast, the other pathological findings showed no association with dental pathology and/or treatment.
In summary, the results of this review demonstrate remarkable evidence for a relationship between maxillary sinus pathology and, particularly, sinus mucosa thickening and the presence of dental modifications in CBCT images. However, although most studies describe an association between sinus pathology and dental pathology, the most frequently observed dental aetiologies are inconsistent. Finally, we found that the presence of an inflammatory sinus pathology, and specifically the thickening of the mucosa of the maxillary sinus, correlates positively and significantly with dental pathology and/or treatment.
LIMITATIONS
The aim of this study was to review the data available in the literature on odontogenic maxillary sinus pathology. The results highlight the importance of dental modifications, observed by means of CBCT, as a frequent cause of maxillary sinusitis, offering a new perspective on the pathology of the maxillary sinus. However, the study has a number of limitations.
Selection bias is one of the most important aspects to be addressed in a review article. For this review, we selected studies that included CBCT images of otolaryngology patients with maxillary sinusitis and dental patients with or without dental and/or sinus pathology. One limitation is the existence of possible confounding factors resulting from the heterogeneous characteristics of the patients.
Other limitations are linked to the very nature of the case series, cross-sectional and case-control studies, which have inherent bias in their retrospective design. In addition, we did not assess the methodological quality of the selected studies.
Finally, due to the heterogeneity of the data collected from the included studies, it was not possible to perform a meta-analysis on the prevalence of odontogenic maxillary sinusitis.
CONCLUSIONS
The incidence of sinusitis of dental origin is probably underestimated in the available literature. The most recent studies suggest a much higher incidence, close to 30-40 % of all cases of chronic maxillary sinusitis. Inflammatory processes and, in particular, the thickening of the mucosa of the maxillary sinus are frequently related to the presence of dental modifications observed in CBCT images, either due to pathologies or complications after dental treatment. However, given the heterogeneity of the studies included in this review, it was not possible to estimate the prevalence of maxillary sinusitis originating from dental pathologies and/or treatments.
Inflammatory-type alterations of the maxillary sinus account for approximately three thirdsof all pathological findings observed on CBCT images. We also identified infections, tumours and the presence of high pneumatisation in the maxillary sinus, although at a lower frequency. In contrast, other possible causes of sinus pathology, such as iatrogeny, the presence of foreign bodies, and low pneumatisation are very rare in the work included in this review. The majority of the studies agree on an association between maxillary sinus pathology and dental pathology, but diverge in terms of the dental causes most commonly observed in patients with maxillary sinusitis. The dental disorders most frequently associated with sinus pathology are periapical inflammatory cysts and periodontal bone loss.
In conclusion, our results further support the argument that dental modifications and treatments are an important cause of sinus pathology. For this reason, dental aetiologies must be taken into account by both dentists and maxillofacial surgeons when considering the most appropriate treatment for patients with maxillary sinusitis.
REFERENCES
1.Kim H-J, Yoon H-R, Kim K-D, Kang M-K, Kwak H-H, Park H-D, et al. Personal- computer-based three-dimensional reconstruction and simulation of maxillary sinus. Surg Radiol Anat. 2003;24(6):393–9
2.Delgadillo Ávila JR. Growt and development of the maxillary sinus and its relation with the dental roots. Kiru. 2005;2(1):46–51.
3.Patel NA, Ferguson BJ. Odontogenic sinusitis: An ancient but under-appreciated cause of maxillary sinusitis. Curr Opin Otolaryngol Head Neck Surg. 2012;20(1):24–8.
4.Heider C-C, Ribalta L-G, Bacigalupe R-D, Krauss M-K. Rinosinusitis maxilar crónica de origen dental. Rev Otorrinolaringol y cirugía cabeza y cuello. 2014;74(1):12–20.
5.Kretzschmar DP, Kretzschmar CJL. Rhinosinusitis: Review from a dental perspective. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(2):128–35.
6.Pardal-Peláez B, Pardal-Refoyo JL, Montero J, González-Serrano J, López-Quiles J. Classification of sinonasal pathology associated with dental pathology or dental treatment. Minerva Dent Oral Sci. 2021;70(2):71-77.
7.Arias-Irimia O, Barona-Dorado C, Santos-Marino JA, Martínez-Rodríguez N, Martínez-González JM. Meta-analisis of the etiology of odontogenic maxillary sinusitis. Med Oral Patol Oral Cir Bucal. 2010;15(1):3–6.
8.Shiki K, Tanaka T, Kito S, Wakasugi-Sato N, Matsumoto-Takeda S, Oda M, et al. The significance of cone beam computed tomography for the visualization of anatomical variations and lesions in the maxillary sinus for patients hoping to have dental implant-supported maxillary restorations in a private dental office in Japan. Head Face Med. 2014;10(1):1–13.
9.Guijarro-Martínez R, Swennen GRJ. Cone-beam computerized tomography imaging and analysis of the upper airway: A systematic review of the literature. Int J Oral Maxillofac Surg. 2011;40(11):1227–37.
10. Little RE, Long CM, Loehrl TA, Poetker DM. Odontogenic sinusitis: A review of the current literature. Laryngoscope Investig Otolaryngol. 2018;3(2):110–4.
11. Cabezón A R, Vaidés S R, Breinbauer K H, Ramírez R C, Grau L C, Iñíguez CR. Variantes anatómicas relevantes en tomografía computarizada de cavidades perinasales. Rev Otorrinolaringol y cirugía cabeza y cuello. 2010;70(3):223–30.
12. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097.
13. Gutiérrez Mesa M, León-Manco RA, Ruiz García VE. Frecuencia de patología de los senos maxilares evaluados mediante tomografía computarizada de haz cónico. Rev Estomatológica Hered. 2018;28(3):177.
14. Nair S. Correlation between symptoms and radiological findings in patients of chronic rhinosinusitis: A modified radiological typing system. Rhinology. 2009;47(2):181–6.
15. Tezer MS, Tahamiller R, Çanakçioǧlu S. Computed tomography findings in chronic rhinosinusitis patients with and without allergy. Asian Pacific J Allergy Immunol. 2006;24(2–3):123–7.
16. Rose GE, Sandy C, Hallberg L, Moseley I. Clinical and radiologic characteristics of the imploding antrum, or «silent sinus,» syndrome. Ophthalmology. 2003;110(4):811–8.
17. Rózyło-Kalinowska I. Imaging diagnostics strategy in maxillary sinus neoplasms. Ann Univ Mariae Curie-Skłodowska Sect D Med. 2001;56(6):423–9.
18. Krennmair G, Lenglinger F. Maxillary sinus aspergillosis. J Oral Maxillofac Surg. 1995;53(6):657–63.
19. Guerra-Pereira I, Vaz P, Faria-Almeida R, Braga AC, Felino A. CT maxillary sinus evaluation-a retrospective cohort study. Med Oral Patol Oral Cir Bucal. 2015;20(4):e419–26.
20. Costa F, Emanuelli E, Robiony M. Incidence of maxillary sinus disease before sinus floor elevation surgery as identified by cone-beam computedtomography: A literature review. J Oral Implantol. 2018;44(2):161–6.
21. Aksoy U. Association between odontogenic conditions and maxillary sinus mucosal thickening: a retrospective CBCT study. Clin Oral Investig. 2019;23(1):123–31.
22. Avsever H, Gunduz K, Karakoç O, Akyol M, Orhan K. Incidental findings on cone-beam computed tomographic images: paranasal sinus findings and nasal septum variations. Oral Radiol. 2018;34(1):40–8.
23. Kalavagunta S, Reddy KTV. Extensive maxillary sinus pneumatization. Rhinology. 2003;41(2):113–7.
24. Kawai T, Tanaka R, Yeung AWK, von Arx T, Bornstein MM. Frequency and type of incidentally detected radiodensities in the maxillary sinus: a retrospective analysis using cone beam computed tomography (CBCT). Clin Oral Investig. 2019;23(3):1091–9.
25. Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone-beam computed tomography evaluation of maxillary sinusitis. J Endod. 2011;37(6):753–7.
26. Nascimento EHL, Pontual MLA, Pontual AA, Freitas DQ, Perez DEC, Ramos-Perez FMM. Association between Odontogenic Conditions and Maxillary Sinus Disease: A Study Using Cone-beam Computed Tomography. J Endod. 2016;42(10):1509–15.
27. Nunes CABCM, Guedes OA, Alencar AHG, Peters OA, Estrela CRA, Estrela C. Evaluation of Periapical Lesions and Their Association with Maxillary Sinus Abnormalities on Cone-beam Computed Tomographic Images. J Endod. 2016;42(1):42–6.
28. Pazera P, Bornstein MM, Pazera A, Sendi P, Katsaros C. Incidental maxillary sinus findings in orthodontic patients: A radiographic analysis using cone-beam computed tomography (CBCT). Orthod Craniofacial Res. 2011;14(1):17–24.
29. Phothikhun S, Suphanantachat S, Chuenchompoonut V, Nisapakultorn K. Cone-Beam Computed Tomographic Evidence of the Association Between Periodontal Bone Loss and Mucosal Thickening of the Maxillary Sinus. J Periodontol. 2012;83(5):557–64.
30. Pokorny A, Tataryn R. Clinical and radiologic findings in a case series of maxillary sinusitis of dental origin. Int Forum Allergy Rhinol. 2013;3(12):973–9.
31. Roque-Torres GD, Meneses-López A, Bóscolo N, De Almeida SM, Neto FH. Ene-Mar; Rev Estomatol Herediana. 2015;25(1):60-77
32. Rudralingam M, Jones K, Woolford TJ. The unilateral opaque maxillary sinus on computed tomography. Br J Oral Maxillofac Surg. 2002;40(6):504–7.
33. Bajoria AA, Sarkar S, Sinha P. Evaluation of Odontogenic Maxillary Sinusitis with Cone Beam Computed Tomography: A Retrospective Study with Review of Literature. J Int Soc Prev Community Dent. 2019;9(2):194-204.
34. Selcuk A, Ozcan KM, Akdogan O, Bilal N, Dere H. Variations of maxillary sinus and accompanying anatomical and pathological structures. J Craniofac Surg. 2008;19(1):159–64.
35. Tassoker M. What are the risk factors for maxillary sinus pathologies? A CBCT study. Oral Radiol. 2020;36(1):80–4.
36. Troeltzsch M, Pache C, Troeltzsch M, Kaeppler G, Ehrenfeld M, Otto S, et al. Etiology and clinical characteristics of symptomatic unilateral maxillary sinusitis: A review of 174 cases. J Cranio-Maxillofacial Surg. 2015;43(8):1522–9.
37. Lawson W, Patel ZM, Lin FY. The development and pathologic processes that influence maxillary sinus pneumatization. Anat Rec. 2008;291(11):1554–63.
38. Yalcin ED, Akyol S. Relationship Between the Posterior Superior Alveolar Artery and Maxillary Sinus Pathology: A Cone-Beam Computed Tomography Study. J Oral Maxillofac Surg. 2019;77(12):2494–502.
39. Bornstein M, Yeung A, Tanaka R, von Arx T, Jacobs R, Khong P-L. Evaluation of Health or Pathology of Bilateral Maxillary Sinuses in Patients Referred for Cone Beam Computed Tomography Using a Low-Dose Protocol. Int J Periodontics Restorative Dent. 2018;38(5):699–710.
40. Chen HJ, Chen H Sen, Chang YL, Huang YC. Complete unilateral maxillary sinus opacity in computed tomography. J Formos Med Assoc.2010;109(10):709–15.
41. Connor SEJ, Chavda S V., Pahor AL. Computed tomography evidence of dental restoration as aetiological factor for maxillary sinusitis. J Laryngol Otol. 2000;114(7):510–3.
42. Dobele I, Kise L, Apse P, Kragis G, Bigestans A. Radiographic assessment of findings in the maxillary sinus using cone-beam computed tomography. Stomatologija. 2013;15(4):119–22.
43. Drăgan E, Rusa O, Nemţoi A, Melian G, Mihai C, Haba D. Maxillary sinus anatomic and pathologic CT findings in edentulous patients scheduled for sinus augmentation. Rev medico-chirurgicală a Soc Medici şi̧ Nat din Iaşi̧. 2014;118(4):1114–21.
44. Drage N, Rogers S, Greenall C, Playle R. Incidental findings on cone beam computed tomography in orthodontic patients. J Orthod. 2013;40(1):29–37.
45. Horwitz Berkun R, Polak D, Shapira L, Eliashar R. Association of dental and maxillary sinus pathologies with ear, nose, and throat symptoms. Oral Dis. 2018;24(4):650-656.
46. Da Silva AF, Fróes GR Jr, Takeshita WM, Da Fonte JB, De Melo MF, Sousa Melo SL. Prevalence of pathologic findings in the floor of the maxillary sinuses on cone beam computed tomography images. Gen Dent. 2017;65(2):28-32.
47. Ani CC, Adoga AA, Tawe GS. Incidental maxillary sinus findings on cranial computerized tomographic scan in a tropical setting. J West African Coll Surg. 2016;6(2):39–51.
48. Cavalcanti MC, Guirado TE, Sapata VM, et al. Maxillary sinus floor pneumatization and alveolar ridge resorption after tooth loss: a cross-sectional study. Braz Oral Res. 2018;32:e64.
49. Goller-Bulut D, Sekerci AE, Köse E, Sisman Y. Cone beam computed tomographic analysis of maxillary premolars and molars to detect the relationship between periapical and marginal bone loss and mucosal thickness of maxillary sinus. Med Oral Patol Oral Cir Bucal. 2015;20(5):e572–9.
50. Hsiao YJ, Yang J, Resnik RR, Suzuki JB. Prevalence of Maxillary Sinus Pathology Based on Cone-Beam Computed Tomography Evaluation of Multiethnicity Dental School Population. Implant Dent. 2019;28(4):356–66.
51. Manji A, Faucher J, Resnik RR, Suzuki JB. Prevalence of maxillary sinus pathology in patients considered for sinus augmentation procedures for dental implants. Implant Dent. 2013;22(4):428–35.
52. Raghav M, Karjodkar FR, Sontakke S, Sansare K. Prevalence of incidental maxillary sinus pathologies in dental patients on cone-beam computed tomographic images. Contemp Clin Dent. 2014;5(3):361–5.
53. Ritter L, Lutz J, Neugebauer J, Scheer M, Dreiseidler T, Zinser MJ, et al. Prevalence of pathologic findings in the maxillary sinus in cone-beam computerized tomography. Oral Surgery, Oral Med Oral Pathol Oral Radiol Endodontology [Internet]. 2011;111(5):634–40.
54. Tadinada A, Jalali E, Al-Salman W, Jambhekar S, Katechia B, Almas K. Prevalence of bony septa, antral pathology, and dimensions of the maxillary sinus from a sinus augmentation perspective: A retrospective cone-beam computed tomography study. Imaging Sci Dent. 2016;46(2):109–15.
55. Dedeoğlu N, Altun O. Evaluation of maxillary sinus anatomical variations and pathologies in elderly, young, posterior dentate and edentulous patient groups with cone-beam computed tomography. Folia Morphol. 2019;78(3):595–9.
56. Dagassan-Berndt DC, Zitzmann NU, Lambrecht JT, Weiger R, Walter C. Is the Schneiderian membrane thickness affected by periodontal disease? A cone beam computed tomography-based extended case series. J Int Acad Periodontol. 2013;15(3):75–82.
57. Yeung AWK, Tanaka R, Khong PL, von Arx T, Bornstein MM. Frequency, location, and association with dental pathology of mucous retention cysts in the maxillary sinus. A radiographic study using cone beam computed tomography (CBCT). Clin Oral Investig. 2018;22(3):1175–83.
58. Constantine S, Clark B, Kiermeier A, Anderson PP. Panoramic radiography is of limited value in the evaluation of maxillary sinus disease. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;127(3):237-246.
59. Terlemez A, Tassoker M, Kizilcakaya M, Gulec M. Comparison of cone-beam computed tomography and panoramic radiography in the evaluation of maxillary sinus pathology related to maxillary posterior teeth: Do apical lesions increase the risk of maxillary sinus pathology? Imaging Sci Dent. 2019;49(2):115–22.
60. Kaplan BA, Kountakis SE. Diagnosis and pathology of unilateral maxillary sinus opacification with or without evidence of contralateral disease. Laryngoscope. 2004;114(6):981–5.
61. Taher MM, Haddad OS. CT scan findings of occult sinus pathology in asymptomatic individuals. Ann Saudi Med. 1992;12(5):456-458.
Table 1. Counts and general characteristics included in the articles.
Author/year |
Type of study |
Period of study |
Average age |
No. Patients M/f |
No. Maxillary sinuses |
No. Physiological sinuses |
No. Pathological sinuses |
Dental pathology |
Dental treatment |
Aksoy et al., 2018 |
Case series |
2012-2016 |
46.7 |
151M/143F |
588 |
323 |
265 |
224 |
143 |
Almeida et al., 2015 |
Cross-sectional |
2009-2011 |
52 |
194M/306F |
1,000 |
517 |
483 |
No data |
No data |
Ani et al., 2016 |
Cross-sectional |
2015-2015 |
47.5 |
72M/49F |
242 |
196 |
46 |
No data |
No data |
Avsever et al., 2017 |
Case series |
2011-2015 |
45 |
423M/268F |
1,382 |
690 |
692 |
No data |
No data |
Bajoria et al., 2019 |
Case series |
2017-2018 |
40 |
314M/186F |
1,000 |
606 |
394 |
132 |
197 |
Bornstein et al., 2018 |
Case series |
2016-2016 |
32 |
43M/91F |
268 |
169 |
99 |
18 |
3 |
Cavalcanti et al., 2018 |
Cross-sectional |
No data |
47.4 |
74M/109F |
366 |
323 |
43 |
No data |
No data |
Chen et al., 2010 |
Case series |
2004-2008 |
48.1 |
60M/56F |
232 |
116 |
116 |
No data |
No data |
Connor et al., 2000 |
Case series |
1993-1998 |
44.75 |
162M/158F |
330 |
104 |
226 |
No data |
192 |
Constantine et al., 2018 |
Cohort |
No data |
52.85 |
312M/402F |
1,322 |
249 |
1,073 |
No data |
No data |
Dedeoğlu et al., 2019 |
Case-control |
2011-2017 |
45.17 |
66M/74F |
258 |
150 |
108 |
No data |
No data |
Dobele et al., 2013 |
Case series |
No data |
52.53 |
18M/16F |
68 |
35 |
33 |
No data |
No data |
Dorothea et al., 2013 |
Case-control |
2007-2010 |
62.2 |
19M/19F |
76 |
0 |
76 |
17 |
No data |
Drăgan et al., 2014 |
Case series |
No data |
62 |
67M/53F |
240 |
88 |
152 |
No data |
No data |
Drage et al., 2013 |
Case series |
2009-2011 |
14.5 |
145M/184F |
584 |
474 |
110 |
120 |
No data |
Goller-Bulut et al., 2015 |
Cross-sectional |
No data |
38.8 |
101M/104F |
410 |
410 |
0 |
159 |
No data |
Gutierrez Mesa et al., 2018 |
Cross-sectional |
2016-2016 |
47.04 |
116M/254F |
740 |
463 |
277 |
No data |
No data |
Horwitz et al., 2017 |
Case series |
2013-2015 |
55 |
35M/46F |
162 |
48 |
114 |
23 |
No data |
Hsiao et al., 2019 |
Cross-sectional |
2009-2013 |
48.53 |
320M/360F |
1,360 |
998 |
362 |
No data |
No data |
Kalavagunta et al., 2003 |
Case series |
2001-2001 |
No data |
No data |
400 |
364 |
36 |
No data |
No data |
Kaplan et al., 2004 |
Prospective |
1999-2001 |
47 |
30M/34F |
128 |
48 |
80 |
No data |
No data |
Kawai et al., 2018 |
Case series |
2016-2017 |
28.7 |
61M/108F |
338 |
303 |
35 |
19 |
12 |
Maillet et al., 2011 |
Case series |
2006-2008 |
57.3 |
49M/33F |
164 |
29 |
135 |
100 |
21 |
Manji et al., 2013 |
Cross-sectional |
No data |
54.8 |
115M/160F |
550 |
303 |
247 |
No data |
No data |
Nascimento et al., 2016 |
Case series |
2010-2011 |
47.09 |
182M/218F |
766 |
108 |
658 |
580 |
234 |
Nunes et al., 2015 |
Case series |
2009-2013 |
41.2 |
75M/125F |
321 |
178 |
143 |
92 |
No data |
Pazera et al., 2010 |
Case series |
2006-2008 |
17.5 |
63M/76F |
139 |
74 |
65 |
No data |
No data |
Phothikhun et al., 2012 |
Case series |
2009-2009 |
46.1 |
110M/140F |
500 |
304 |
196 |
539 |
21 |
Pokorny et al., 2013 |
Case series |
2010-2012 |
48 |
11M/20F |
33 |
0 |
33 |
24 |
No data |
Raghav et al., 2015 |
Cross-sectional |
No data |
32.09 |
110M/91F |
402 |
162 |
240 |
No data |
38 |
Ritter et al., 2011 |
Cross-sectional |
No data |
44.19 |
533M/493F |
2,058 |
1,403 |
655 |
No data |
No data |
Roque-Torres et al., 2016 |
Case series |
No data |
22 |
31M/78F |
218 |
142 |
76 |
0 |
0 |
Rudralingam et al., 2002 |
Case series |
No data |
No data |
No data |
744 |
744 |
0 |
No data |
No data |
Selcuk et al., 2008 |
Case series |
2006-2007 |
No data |
No data |
660 |
509 |
151 |
No data |
No data |
Tadinada et al., 2016 |
Cross-sectional |
2008-2013 |
53.2 |
17M/19F |
72 |
49 |
23 |
No data |
No data |
Taher et al., 1992 |
Retrospective |
No data |
36 |
62M/52F |
228 |
214 |
14 |
No data |
No data |
Tassoker et al., 2019 |
Case series |
2013-2018 |
32.93 |
76M/124F |
400 |
215 |
185 |
141 |
No data |
Terlemez et al., 2019 |
Cohort |
No data |
28.58 |
111M/174F |
570 |
327 |
243 |
157 |
112 |
Troeltzsch et al., 2015 |
Case series |
2006-2013 |
52.7 |
102M/72F |
174 |
0 |
174 |
150 |
150 |
Wai et al., 2017 |
Case-control |
2016-2017 |
29 |
53M/103F |
310 |
270 |
40 |
No data |
No data |
William et al., 2008 |
Case series |
No data |
No data |
No data |
5,080 |
4,955 |
125 |
No data |
No data |
Yalcin et al., 2019 |
Case series |
2015-2017 |
34.72 |
155M/170F |
650 |
258 |
392 |
No data |
No data |
F: Female; M: Male |
|||||||||
Table 4. Sinus findings grouped into subgroups.
AUTHOR/YEAR |
INFLAMMATION |
INFECTION |
TUMOUR |
LOW PNEUMATISATION |
HIGH PNEUMATISATION |
FOREIGN BODY |
SYMPTOMS |
IATROGENY |
TOTAL FINDINGS |
Aksoy et al., 2018 |
265 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
265 |
Almeida et al., 2015 |
406 |
No data |
71 |
No data |
No data |
6 |
No data |
No data |
483 |
Ani et al., 2016 |
17 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
17 |
Avsever et al., 2017 |
605 |
No data |
25 |
24 |
No data |
No data |
No data |
No data |
654 |
Bajoria et al., 2019 |
No data |
387 |
6 |
No data |
No data |
1 |
No data |
No data |
394 |
Bornstein et al., 2018 |
52 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
52 |
Cavalcanti et al., 2018 |
No data |
No data |
No data |
No data |
181 |
No data |
No data |
No data |
181 |
Chen et al., 2010 |
3 |
95 |
18 |
No data |
No data |
No data |
No data |
No data |
116 |
Connor et al., 2000 |
48 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
48 |
Constantine et al., 2018 |
776 |
153 |
155 |
No data |
No data |
No data |
No data |
4 |
1,088 |
Dedeoğlu et al., 2019 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
108 |
108 |
Dobele et al., 2013 |
53 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
53 |
Dorothea et al., 2013 |
76 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
76 |
Drăgan et al., 2014 |
68 |
No data |
2 |
No data |
No data |
No data |
No data |
No data |
70 |
Drage et al., 2013 |
79 |
No data |
23 |
3 |
No data |
5 |
No data |
No data |
110 |
Goller-Bulut et al., 2015 |
766 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
766 |
Gutierrez Mesa et al., 2018 |
277 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
277 |
Horwitz et al., 2017 |
113 |
0 |
No data |
No data |
No data |
No data |
57 |
No data |
170 |
Hsiao et al., 2019 |
357 |
No data |
No data |
No data |
No data |
5 |
No data |
No data |
362 |
Kalavagunta et al., 2003 |
No data |
163 |
No data |
5 |
16 |
No data |
No data |
No data |
184 |
Kaplan et al., 2004 |
28 |
29 |
7 |
No data |
No data |
No data |
No data |
No data |
64 |
Kawai et al., 2018 |
77 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
77 |
Maillet et al., 2011 |
No data |
135 |
No data |
No data |
No data |
No data |
No data |
No data |
135 |
Manji et al., 2013 |
124 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
124 |
Nascimento et al., 2016 |
592 |
42 |
24 |
No data |
No data |
No data |
No data |
No data |
658 |
Nunes et al., 2015 |
76 |
No data |
6 |
No data |
No data |
5 |
No data |
No data |
87 |
Pazera et al., 2010 |
60 |
5 |
No data |
No data |
No data |
No data |
No data |
No data |
65 |
Phothikhun et al., 2012 |
146 |
No data |
50 |
No data |
No data |
No data |
No data |
No data |
196 |
Pokorny et al., 2013 |
6 |
26 |
1 |
No data |
No data |
No data |
No data |
No data |
33 |
Raghav et al., 2015 |
237 |
No data |
No data |
No data |
No data |
3 |
No data |
No data |
240 |
Ritter et al., 2011 |
588 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
588 |
Roque-Torres et al., 2016 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
0 |
Rudralingam et al., 2002 |
360 |
4 |
6 |
No data |
No data |
No data |
No data |
No data |
370 |
Selcuk et al., 2008 |
100 |
No data |
No data |
31 |
3 |
No data |
No data |
No data |
134 |
Tadinada et al., 2016 |
4 |
No data |
19 |
No data |
No data |
No data |
No data |
No data |
23 |
Taher et al., 1992 |
14 |
No data |
2 |
No data |
No data |
No data |
No data |
No data |
16 |
Tassoker et al., 2019 |
141 |
No data |
No data |
No data |
No data |
44 |
No data |
No data |
185 |
Terlemez et al., 2019 |
243 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
243 |
Troeltzsch et al., 2015 |
174 |
136 |
21 |
No data |
No data |
3 |
No data |
60 |
394 |
Wai et al., 2017 |
29 |
No data |
56 |
No data |
No data |
No data |
No data |
No data |
85 |
William et al., 2008 |
No data |
No data |
101 |
1 |
No data |
No data |
No data |
No data |
102 |
Yalcin et al., 2019 |
319 |
No data |
73 |
No data |
No data |
No data |
No data |
No data |
392 |
TOTAL |
7,279 |
1,175 |
666 |
64 |
200 |
72 |
57 |
172 |
9,685 |